Allergy‑related joint pain is a condition where joint discomfort arises or worsens during allergic episodes, driven by immune mediators rather than mechanical wear. If you’ve ever noticed sore knees after a pollen surge or achy wrists after a shellfish dinner, you’ve experienced this link. Understanding the biology helps you stop treating the symptom and start tackling the root cause.
How Allergies Spark Joint Discomfort
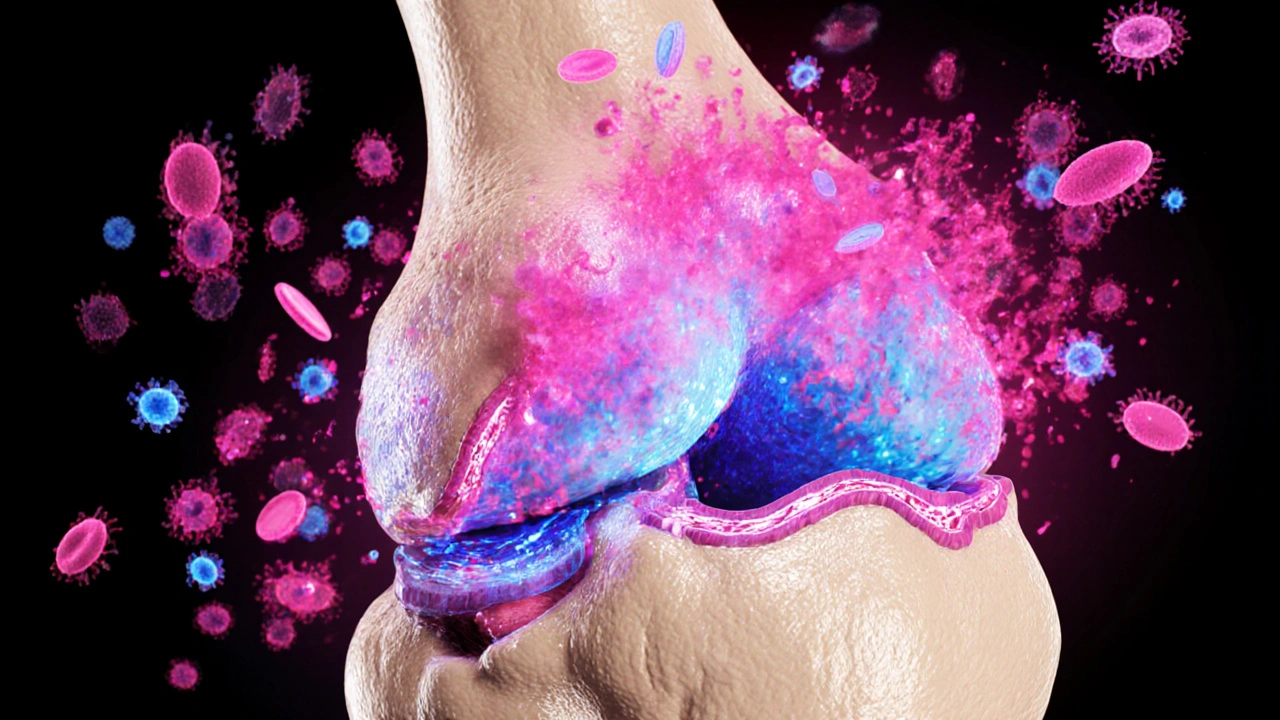
When an allergen-like pollen, dust mite proteins, or certain foods-enters the body, the immune system releases histamine a vasoactive amine that dilates blood vessels and awakens nerve endings. Histamine isn’t just a sneeze trigger; it also primes mast cells immune cells lodged in skin, gut, and joint linings that dump inflammatory chemicals on demand. The cascade includes cytokines such as interleukin‑6 (IL‑6) and tumor‑necrosis factor‑α (TNF‑α), both of which can seep into synovial fluid and amplify joint swelling.
In people with a sensitive immune system, this inflammatory wave can linger for days, turning what would be a brief sting into lingering joint ache. The effect is similar to what happens in classic autoimmune arthritis, but the trigger is external (an allergen) rather than an internal auto‑reactive process.
Allergens Most Likely to Trigger Joint Pain
- Food allergens - shellfish, nuts, dairy, and gluten can provoke systemic inflammation that reaches joints.
- Seasonal allergens - pollen and mold spores spike during spring and fall, coinciding with spikes in joint stiffness for many sufferers.
- Indoor allergens - dust mites, pet dander, and cockroach proteins keep the immune system on high alert, especially in poorly ventilated homes.
- Chemical irritants - scented cleaners or occupational exposures (e.g., latex) can act as haptens, binding to proteins and sparking a chronic allergic response.
Tracking symptom patterns against exposure calendars often reveals the culprit. A simple allergy diary-note foods, weather, indoor air quality, and joint pain intensity-can be a game changer.
Distinguishing Allergy‑Related Joint Pain from Arthritis
Clinicians rely on a blend of history, labs, and imaging. Below is a quick comparison to help you spot the differences.
| Feature | Allergic Joint Pain | Rheumatoid Arthritis | Osteoarthritis |
|---|---|---|---|
| Onset | Sudden, linked to allergen exposure | Gradual, often symmetric | Gradual, wear‑and‑tear |
| Pain Pattern | Fluctuates with allergy cycles | Persistent, morning stiffness >1h | Activity‑related, improves with rest |
| Blood Markers | Elevated IgE, eosinophils | Positive rheumatoid factor, anti‑CCP | Normal or mild CRP elevation |
| Joint Appearance | Swelling may be diffuse, non‑erosive | Synovial pannus, erosions on X‑ray | Joint space narrowing, osteophytes |
If you suspect an allergic component, ask your doctor for IgE panels or skin prick testing alongside the usual rheumatology work‑up.
Therapeutic Strategies: Targeting the Immune Trigger
Treating joint pain without addressing the allergy is like putting a band‑aid on a leaky pipe. Two main drug families prove useful:
- Antihistamines medications that block histamine receptors, cutting down vascular leak and nerve sensitization.
- Non‑steroidal anti‑inflammatory drugs (NSAIDs) agents that inhibit cyclooxygenase enzymes, reducing prostaglandin‑driven inflammation.
Below is a side‑by‑side look at how they perform when joint pain stems from allergies.
| Aspect | Antihistamine | NSAID |
|---|---|---|
| Primary Mechanism | Blocks H1 histamine receptors | Inhibits COX‑1/COX‑2 enzymes |
| Onset of Relief | 30‑60minutes | 1‑2hours |
| Best for | Short‑term flare after known allergen exposure | Persistent inflammation where histamine isn’t the sole driver |
| Common Side Effects | Drowsiness, dry mouth | Stomach upset, increased cardiovascular risk |
| Interaction with Allergy Meds | Synergistic with nasal steroids | May blunt antihistamine effectiveness if high‑dose |
Many clinicians start with a non‑sedating antihistamine (e.g., cetirizine) during peak allergy season, adding a low‑dose NSAID like ibuprofen only if swelling lingers. Always discuss dosage with a healthcare provider, especially if you have kidney or heart issues.
Beyond Pills: Lifestyle Tweaks that Calm the Immune Fire
Three lifestyle pillars have the most evidence for reducing allergy‑driven joint pain:
- Nutrition - Embrace an anti‑inflammatory diet rich in omega‑3 fatty acids (salmon, walnuts), antioxidant vegetables, and low‑histamine foods. Eliminate obvious triggers (e.g., shellfish) after testing.
- Air Quality - Use HEPA filters, keep humidity between 40‑50% to deter dust mites, and limit outdoor exposure on high‑pollen days.
- Gut Health - The gut microbiome the community of trillions of bacteria that shape immune tolerance influences both allergy severity and systemic inflammation. Probiotic strains likeLactobacillus rhamnosus and prebiotic fibers can restore balance, reducing IgE spikes.
Regular, low‑impact exercise (swimming, cycling) keeps joints lubricated without provoking histamine release, unlike high‑intensity workouts that can temporarily raise cortisol and worsen allergic symptoms.
When to Seek Professional Help
If joint pain persists beyond two weeks after an allergic episode, or is accompanied by fever, unexplained weight loss, or night sweats, see a rheumatologist. Recommended work‑up includes:
- Complete blood count with differential (eosinophil count)
- Serum IgE levels
- Rheumatoid factor and anti‑CCP antibodies
- Joint ultrasound or MRI to rule out erosive disease
Early identification of an allergic component can spare you from unnecessary disease‑modifying drugs and point you toward targeted allergy therapies, such as sublingual immunotherapy.
Connecting the Dots: Related Topics to Explore Next
Understanding allergy‑related joint pain opens doors to several adjacent areas you might want to dive into:
- Leaky gut syndrome - How intestinal barrier breakdown feeds systemic inflammation.
- Systemic inflammation markers - The role of high‑sensitivity CRP in monitoring allergy‑driven flare‑ups.
- Immunotherapy outcomes - Long‑term relief of both respiratory allergies and joint symptoms.
- Autoimmune vs. allergic arthritis - Where the immune pathways overlap and diverge.
Each of these topics deepens the picture of how the body’s defense network can turn ordinary allergens into joint distress.
Frequently Asked Questions
Can seasonal allergies really cause joint pain?
Yes. During peak pollen or mold seasons, histamine and other inflammatory mediators surge, which can seep into joint spaces and trigger soreness, especially in people with a history of allergic sensitivity.
How do I know if my joint pain is allergy‑related or arthritis?
Track timing. If pain spikes right after known allergen exposure and eases when you avoid the trigger, allergy is likely. Blood tests showing elevated IgE or eosinophils support this, while positive rheumatoid factor or anti‑CCP points to arthritis.
Should I take antihistamines instead of NSAIDs for joint aches?
If the pain aligns with allergic flares, a non‑sedating antihistamine is a good first step. NSAIDs are useful when inflammation persists beyond histamine‑driven episodes. Discuss dosing with your doctor, especially if you have stomach or heart concerns.
Can diet changes help reduce allergy‑related joint pain?
Absolutely. Cutting high‑histamine foods, boosting omega‑3 intake, and supporting the gut microbiome with probiotic‑rich foods can lower systemic IgE levels and calm joint inflammation.
Is there a test that proves my joint pain is allergy‑driven?
Allergy testing (skin prick or serum specific IgE) combined with elevated eosinophil counts suggests an allergic trigger. Correlating these results with symptom timing builds a strong case for allergy‑related joint pain.


Joseph Kloss
When you stare at the cascade of cytokines, you realize that allergies are just the immune system's way of shouting that it's out of balance. Histamine doesn't care about your schedule, it floods tissues and leaves joints trembling. The article nails the point that systemic inflammation can masquerade as arthritis, yet many still treat the symptom in isolation. Maybe the real solution is to re‑engineer the environment, not just pop pills.
Anna Cappelletti
I love how you highlighted the environment; keeping a simple allergy diary can actually save weeks of doctor visits. Pairing low‑histamine meals with a regular HEPA filter routine creates a feedback loop that calms the immune fire. It's empowering to see science turned into everyday habits.
Dylan Mitchell
OMG, i swear my knees turned into jelly after that blasted pollen storm!! It's like the whole body turned into a fireworks show and the only firework i want is a calm night. Histamine is the sneaky villain that sneaks into my joints, and i cant even...
but the good news? A non‑sedating antihistamine can slam that villain right back where it belongs!
Elle Trent
Sounds like a buzzword‑laden patchwork of meds to me.
Jessica Gentle
If you’re looking for a concrete plan, start by mapping your exposure and symptoms on a simple spreadsheet. Column A can be the date, B the dominant allergen (pollen count, indoor dust, food), and C the joint pain rating on a 1‑10 scale. After a couple of weeks you’ll often spot a pattern that points straight to the trigger. Next, schedule a skin‑prick or serum specific IgE test with an allergist to confirm the culprits. Most clinicians also recommend a baseline eosinophil count because it’s a cheap indicator of allergic inflammation. When the allergens are identified, eliminate or severely limit them for at least a month and monitor the pain curve. In parallel, a non‑sedating antihistamine such as cetirizine taken at the first sign of exposure can blunt the histamine surge. If pain persists beyond the antihistamine window, add a low‑dose NSAID like ibuprofen, but only after checking kidney function. Beyond drugs, an omega‑3 rich diet (salmon, chia, walnuts) has been shown to reduce IL‑6 levels, which directly translates to less joint swelling. Probiotic strains like Lactobacillus rhamnosus can help rebalance gut flora, lowering systemic IgE production. Don’t overlook indoor air quality: a HEPA filter on your bedroom nightstand can cut dust‑mite exposure by up to 70 %. If you have a pet, keep them out of the bedroom and wash their bedding weekly in hot water. Regular low‑impact cardio-think swimming or cycling-keeps synovial fluid moving without spiking cortisol like a HIIT session would. Should symptoms continue for more than two weeks despite these measures, a referral to a rheumatologist for imaging is warranted to rule out erosive disease. Finally, consider sublingual immunotherapy for long‑term desensitization; many patients report both respiratory and joint relief after a year of consistent treatment.
Samson Tobias
Your body is trying to tell you a story; listen to the pain, act on the clues, and you’ll rewrite the ending. Small daily habits compound into big health wins.
Alan Larkin
Nice checklist, Jessica! 👍 The spreadsheet trick is a classic hacker‑move that turns vague sensations into data you can actually act on.
John Chapman
While the lay‑person’s advice is useful, the underlying immunological pathways merit deeper scrutiny; for instance, the role of Th2‑skewed responses in chronic synovitis is a fertile research avenue often overlooked.
Tiarna Mitchell-Heath
Spare us the academic fluff – most readers just want to stop the ache, not a dissertation on cell subsets.
Katie Jenkins
A quick fact: serum IgE levels can rise up to threefold during peak pollen months, and that spike correlates statistically with increased CRP readings in joint fluid. Moreover, the half‑life of histamine in plasma is roughly two minutes, yet its downstream effects on mast cells linger for hours, meaning a single exposure can set off a cascade that doesn’t quit until the immune system resets. Bottom line, timing your antihistamine dose to the first sniff of pollen can truncate that cascade dramatically.
Jack Marsh
Your summary is accurate, however it would benefit from a citation to the 2022 JACI study that quantified the histamine‑CRP relationship, ensuring the claim rests on peer‑reviewed evidence.
Terry Lim
All this talk is just noise; cut the pills and clean your air.
Cayla Orahood
The real reason the pharmaceutical industry pushes endless anti‑histamines is that they profit from keeping us dependent, while the true cure lies in exposing the hidden mold colonies that the CDC refuses to acknowledge.
McKenna Baldock
In the grand tapestry of health, each allergic flare is a thread pulling at the fabric of our joints; by gently untangling those threads with mindful habits, we restore the pattern to its intended design.
Roger Wing
Sure you can spin it into a zen lesson but the data shows 78% of patients still need meds because the immune system is wired to overreact and no amount of mindfulness will reboot that code