Calcium Absorption – What It Is and Why It Matters
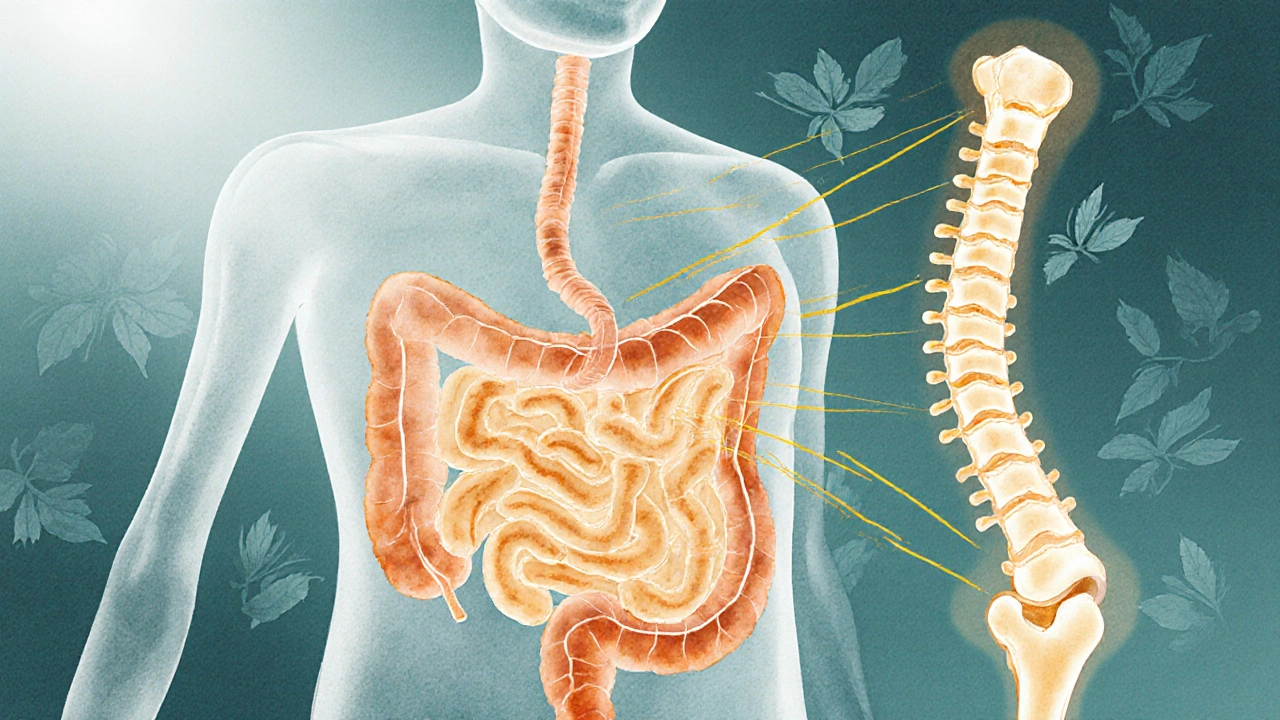
When talking about Calcium Absorption, the process by which the digestive system takes up calcium from food and supplements into the bloodstream. Also known as Calcium Uptake, it is the gateway to strong bones, muscle function, and nerve signaling.
One of the main drivers behind this process is Vitamin D, a fat‑soluble vitamin that enhances calcium uptake in the intestines. Without enough vitamin D, even a diet rich in dairy or fortified foods can leave you with low calcium levels. Another crucial player is Parathyroid Hormone, a hormone that regulates blood calcium by signaling kidneys, bones, and the gut. Together, these entities create a feedback loop: low blood calcium triggers PTH, which then boosts vitamin D activation, improving intestinal absorption.
Key Factors That Influence Calcium Absorption
Age is a big factor. Younger people absorb up to 35 % of the calcium they eat, but that drops to about 15 % after age 50. Hormonal changes, especially reduced estrogen in post‑menopausal women, also blunt the efficiency of the gut. Dietary components matter too—protein and certain acids can help, while excess sodium, caffeine, and phosphates can compete with calcium for transport sites.
Medications can tip the balance. Long‑term glucocorticoids (like prednisone) suppress vitamin D activation, making it harder for the gut to pull calcium in. Some diuretics increase calcium loss through urine, indirectly lowering the amount available for absorption. Even over‑the‑counter antacids that raise stomach pH can reduce calcium solubility, limiting uptake.
On the positive side, certain nutrients act as allies. Magnesium supports the enzymatic steps that convert vitamin D to its active form. Vitamin K2 directs calcium to the skeleton instead of soft tissues, reducing the risk of arterial calcification. Pairing calcium‑rich meals with a little healthy fat improves vitamin D’s effectiveness because it’s fat‑soluble.
Practical tips for maximizing calcium absorption are simple. Aim for 1,000 mg of calcium daily if you’re under 50, and 1,200 mg if you’re older. Split the dose into two meals—your gut can only handle about 500 mg at a time. Choose food sources like low‑fat dairy, leafy greens, fortified plant milks, and tofu. Get 600–800 IU of vitamin D daily through sunlight or a supplement, especially in winter months. Keep sodium under 2,300 mg and limit caffeine to less than 300 mg per day.
Understanding the interplay between calcium, vitamin D, and parathyroid hormone helps you spot why a particular supplement or medication might not be working. If you’re on a steroid regimen, ask your doctor about a higher vitamin D dose or a calcium citrate supplement, which is easier on the stomach. If you have kidney issues, monitoring PTH levels becomes critical, as the hormone can drive bone loss when it stays high for too long.
Below you’ll find a collection of articles that dig deeper into each of these aspects—ranging from how specific drugs affect calcium balance to detailed diet plans for bone health. Whether you’re a teenager building a strong foundation, a middle‑aged adult trying to prevent loss, or a senior focused on maintaining independence, the posts ahead give you science‑backed, actionable advice you can start using right away.
How Poor Food Absorption Triggers Osteoporosis - What You Need to Know
Explore how poor nutrient absorption leads to osteoporosis, identify key gut disorders, and learn practical steps to boost bone health.
More