Bone Health Nutrient Absorption Calculator
Nutrient Absorption Calculator
This tool estimates how gut conditions affect calcium and vitamin D absorption, helping you understand bone health risks.
Estimated Absorption Rates
When your bones become fragile, osteoporosis is the condition that describes this loss of bone density. Most people think of calcium or aging, but the gut plays a starring role. If your body can’t pull the right nutrients from food, the skeleton pays the price. Below you’ll discover why, which disorders matter most, and what you can do to keep your bones strong.
Key Takeaways
- Malabsorption reduces calcium, vitamin D, and other bone‑building nutrients, accelerating bone loss.
- Common gut disorders-celiac disease, Crohn’s disease, chronic pancreatitis, and severe IBS-are linked to higher osteoporosis risk.
- Optimizing gut health, using targeted supplements, and choosing easily absorbable foods can reverse or slow bone deterioration.
- Blood tests for vitamin D, calcium, magnesium, and parathyroid hormone help pinpoint absorption problems.
- Early medical evaluation is crucial when you experience unexplained fractures, frequent falls, or chronic digestive symptoms.
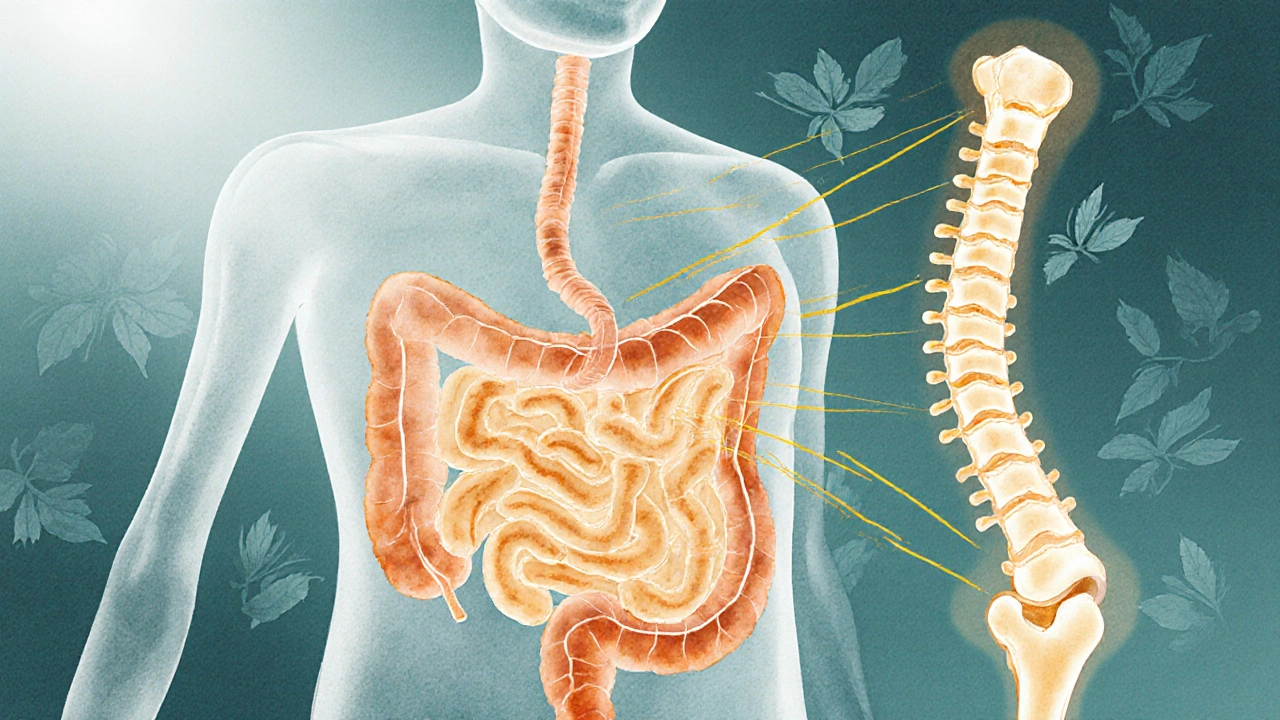
How Malabsorption Undermines Bone Health
The skeleton is a living organ that constantly remodels itself. Osteoclasts break down old bone, while osteoblasts lay down new matrix. This balance depends on a steady supply of minerals (calcium, phosphorus, magnesium) and vitamins (D, K, C). malabsorption is the term for an intestine that fails to extract these nutrients efficiently. When absorption drops, calcium levels in the bloodstream slip, prompting the parathyroid glands to release more parathyroid hormone (PTH). Elevated PTH forces the body to leach calcium from bone, weakening the framework and setting the stage for osteoporosis.
Vitamin D complicates the picture. It acts like a key that unlocks calcium channels in the gut. If you lack enough vitamin D-or if your gut can’t convert it into its active form-calcium stays locked inside the intestinal lumen and never reaches the bloodstream. The result is a double hit: low calcium plus insufficient vitamin D, both of which accelerate bone loss.

Major Conditions That Cause Poor Nutrient Absorption
Not all digestive problems affect bone health equally. The following conditions are the most documented culprits:
| Condition | Primary Nutrient Affected | Typical Bone‑Health Consequence |
|---|---|---|
| Celiac disease | Calcium, vitamin D, iron | Accelerated bone loss, higher fracture risk |
| Crohn’s disease | Calcium, vitamin K, magnesium | Chronic osteopenia, early‑onset osteoporosis |
| Chronic pancreatitis | Fat‑soluble vitamins (D, K, A, E) | Severe calcium deficiency, rapid bone demineralization |
| Small‑intestinal bacterial overgrowth (SIBO) | Vitamin B12, calcium | Subtle bone density decline over years |
| Lactose intolerance (severe) | Calcium from dairy sources | Gradual reduction in bone mineral density |
Each disorder disrupts the gut lining or enzyme production, limiting how much of the vital nutrients reach the bloodstream. In many cases, the damage is reversible with proper treatment, but delayed diagnosis can lock in bone loss that’s hard to recover.
Key Nutrients the Skeleton Craves
Understanding which nutrients matter most helps you target the right foods and supplements.
- Calcium - the building block of bone mineral; adults need about 1,000mg daily, rising to 1,200mg after age50.
- Vitamin D - regulates calcium absorption; optimal serum levels are 30‑50ng/mL. Sun exposure plus 800‑2,000IU of vitamin D₃ daily is common guidance.
- Vitamin K2 - guides calcium to bone rather than arteries; fermented foods and natto provide 90‑120µg per day.
- Magnesium - co‑factor for vitamin D activation; 310‑420mg daily supports bone remodeling.
- Phosphorus - partners with calcium to form hydroxyapatite; excess intake can hinder calcium uptake if not balanced.
When any of these fall short, osteoclast activity outpaces osteoblast formation, and the bone architecture weakens.

Practical Ways to Boost Nutrient Absorption
Improving gut health is a two‑pronged strategy: treat the underlying disorder and adopt dietary habits that enhance absorption.
- Identify and treat the root cause. A gastroenterologist can run blood panels, stool tests, and imaging to pinpoint celiac disease, Crohn’s, or SIBO. Appropriate medication-gluten‑free diet, anti‑inflammatories, antibiotics, pancreatic enzyme replacement-lays the foundation.
- Pair calcium with vitamin D. Consuming fortified dairy or calcium‑rich leafy greens together with a vitamin D source (sunlight, fatty fish, fortified orange juice) maximizes uptake. A 500mg calcium dose with 1,000IU vitamin D improves serum calcium by up to 30% versus calcium alone.
- Include healthy fats. Vitamins D and K are fat‑soluble; a splash of olive oil or a handful of nuts with your greens helps the body absorb them.
- Use probiotics and pre‑biotics. A balanced gut microbiome produces short‑chain fatty acids that strengthen the intestinal lining. Strains such as*Lactobacillus reuteri* have been linked to modest increases in bone density in older adults.
- Space out calcium supplements. The gut can only absorb about 500mg of calcium at a time. Split doses (e.g., 250mg with breakfast and 250mg with dinner) avoids saturation and reduces the risk of kidney stones.
- Avoid interfering substances. Excess caffeine, high‑phytate foods (raw beans, unsoaked grains), and certain medications (PPIs, steroids) can lower calcium absorption. Timing calcium away from these agents helps.
For people with severe malabsorption, prescription‑strength vitamin D₃ (5,000‑10,000IU) and calcium citrate (a form easier on the stomach) are often recommended.
When to Seek Professional Evaluation
If you notice any of the following, schedule a visit with your primary care physician or a bone‑health specialist:
- Unexplained fractures after minor falls.
- Chronic digestive symptoms (bloating, diarrhea, weight loss) lasting more than three months.
- Repeated low bone‑density scans (DXA T‑score ≤‑1.0) despite a calcium‑rich diet.
- Family history of osteoporosis combined with a known gut disorder.
Doctors will typically order a 25‑hydroxy vitamin D test, serum calcium, magnesium, PTH, and possibly a comprehensive stool panel. Results guide personalized supplementation and dietary adjustments.
Frequently Asked Questions
Can a gluten‑free diet prevent osteoporosis?
A gluten‑free diet stops the immune attack on the small intestine in celiac disease, allowing the gut to recover its absorptive surface. Over time, calcium and vitamin D uptake improve, which can slow or reverse bone loss. The diet alone won’t cure existing osteoporosis, but it’s a crucial first step for bone health.
Is calcium citrate better than calcium carbonate for malabsorption?
Calcium citrate requires less stomach acid to dissolve, so it’s absorbed more reliably in people with low acid production or after gastric surgery. In malabsorption cases, many clinicians prefer citrate to maximize the amount that actually reaches the bloodstream.
How much vitamin D should I take if I have Crohn’s disease?
Dosage varies, but studies show that 5,000-10,000IU of vitamin D₃ daily can raise serum 25‑hydroxy levels to the optimal range in most Crohn’s patients. Always confirm with blood tests before high‑dose supplementation.
Do probiotics really improve bone density?
Research in older adults shows that daily intake of*Lactobacillus reuteri* for a year modestly increased lumbar spine bone density (about 1%). The effect is modest but can complement calcium and vitamin D therapy.
What signs indicate my bones are getting weaker?
Frequent fractures from minor bumps, a gradual decrease in height, or a stooped posture (kyphosis) are classic clues. Even if you feel fine, a routine bone‑density scan for anyone over 50 (or younger with risk factors) can catch loss before a break occurs.
Bottom line: if your gut isn’t pulling in calcium, vitamin D, and the other bone‑building nutrients, your skeleton pays the price. By spotting malabsorption early, fixing the underlying gut issue, and feeding your bones with the right nutrients in the right form, you can keep osteoporosis at bay and enjoy a stronger, more resilient body.

johnson mose
Imagine your gut as a bustling market where calcium and vitamin D are the prized goods. When the stalls are damaged by celiac, Crohn’s, or chronic pancreatitis, the merchants can’t hand over their wares, and your bones feel the shortage. That’s why doctors now look beyond dairy and sunshine, digging into the intestinal lining when osteoporosis pops up. Fixing the underlying malabsorption not only boosts the numbers on a DXA scan but also spares you from high‑dose pills that can irritate the stomach. Think of it as a two‑step dance: first, treat the gut; second, feed the skeleton with easily absorbable nutrients.
Most patients see a noticeable lift in serum calcium within weeks of a gluten‑free regimen or enzyme replacement, proving the gut‑bone connection isn’t just theory.
Charmaine De Castro
Thanks for that vivid picture! It’s also worth noting that a simple blood panel for 25‑hydroxy vitamin D and parathyroid hormone can flag absorption issues before any fracture occurs. Pairing a low‑dose calcium citrate with a modest vitamin D3 supplement often does the trick while the gut heals.
Mark Mendoza
From a philosophical standpoint, the body is a micro‑cosm of exchange: what we fail to assimilate internally mirrors what we neglect externally. 🌱 If the intestine refuses to let in the minerals, the skeleton pays the price, echoing the old maxim “you are what you absorb.” Balancing the internal economy with targeted probiotics and split calcium doses can restore harmony. 😊
Dan Tourangeau
Quick tip: split your calcium intake into two 500 mg servings to keep absorption efficient.
Bernard Valentinetti
Ah, but dear Dan, one must not diminish the grandeur of the digestive symphony!; indeed, the mere act of dividing calcium is but a modest overture; the true crescendo arrives when one pairs each dose with a splash of extra‑virgin olive oil, a whisper of fat‑soluble vitamin K2, and perhaps a dash of fermented kimchi to summon the probiotic chorus; thereby the gut not only welcomes calcium but sings it into the bloodstream with operatic vigor! 🎭
Kenneth Obukwelu
Across many cultures, fermented foods like kefir, miso, and natto have long been the secret weapon against bone loss. They supply the friendly bacteria that reinforce the intestinal barrier, allowing calcium and vitamin D to slip through more gracefully. Incorporating these staples can be a flavorful way to protect your skeleton while honoring culinary heritage.
Josephine hellen
When you think about osteoporosis, the first image that often springs to mind is an elderly person with brittle bones, but the story begins much earlier, in the very lining of the small intestine where nutrients are harvested. If that lining is scarred or inflamed-by celiac disease, Crohn’s disease, or even subtle SIBO-the harvest is poor, and the skeleton is starved of the calcium and vitamin D it craves. The cascade starts with low serum calcium, prompting the parathyroid glands to secrete more PTH, which in turn steals calcium from the bones to keep the blood level stable. Over time, this relentless leaching weakens the trabecular architecture, making fractures more likely even with minor falls. The good news is that this process is not irreversible; a targeted approach can turn the tide. First, identify the culprit gut condition through appropriate labs and imaging, because treating the root cause halts further damage. Second, optimize your nutrient intake: choose calcium citrate, which doesn’t rely on high stomach acidity, and split doses to stay under the 500 mg absorption ceiling. Third, ensure you get enough vitamin D-ideally 2,000–5,000 IU daily, depending on baseline levels-to unlock calcium channels in the gut. Fourth, add vitamin K2-rich foods like fermented soy or hard cheeses; K2 directs calcium to bone rather than arteries. Fifth, don’t forget magnesium; it works hand‑in‑hand with vitamin D to activate the enzymes that deposit calcium. Sixth, incorporate healthy fats, such as a drizzle of olive oil or a handful of nuts, because vitamins D and K are fat‑soluble and need a lipid buddy to be absorbed. Seventh, consider a probiotic regimen featuring Lactobacillus reuteri, which has modest evidence for improving bone density in older adults. Eighth, avoid known absorption antagonists-excess caffeine, high‑phytate grains, and certain medications like proton pump inhibitors-by timing your calcium away from them. Ninth, stay active with weight‑bearing exercises; mechanical stress signals the bones to build more matrix, complementing the nutritional strategy. Tenth, monitor your blood work every three to six months, adjusting supplements as needed. Eleventh, engage your healthcare team-gastroenterologists, endocrinologists, and dietitians-to keep the plan coordinated. Lastly, remember that consistency beats intensity; small, daily habits compound over years to produce a sturdier skeleton. By treating the gut and feeding the bones wisely, you can keep osteoporosis at bay and enjoy a life of strength and mobility.
Ria M
Picture the gut as a storm‑tossed sea, with nutrients like tiny ships struggling to reach the distant shore of the bones. When the waves of inflammation crash harder-courtesy of SIBO or chronic pancreatitis-those ships are wrecked, and the skeletal coast erodes. Only by calming the tempest with proper diet, targeted enzymes, and a heroic dose of vitamin D can we hope to rescue the fleet and rebuild the fortress of our frame.
Michelle Tran
Bone health starts in the gut, plain and simple. 😊
Caleb Ferguson
Balancing bone health and gut function isn’t a zero‑sum game; a well‑structured meal plan that includes calcium‑rich leafy greens, fortified plant milks, and a modest amount of oily fish can simultaneously support the microbiome and the skeleton. Regular check‑ups to track vitamin D and magnesium levels help fine‑tune the approach.
Delilah Jones
While your suggestions are solid, let’s not gloss over the fact that many patients ignore the timing of calcium versus their nighttime PPIs, which can blunt absorption dramatically. A simple switch to morning dosing can make a measurable difference.
Pastor Ken Kook
Got to love how a splash of olive oil can turn a boring calcium pill into a gut‑friendly hero. 👍
Jennifer Harris
Interesting how the interplay of PTH and vitamin D creates a feedback loop; tracking both gives a clearer picture of underlying malabsorption.
Northern Lass
One might argue that the prevailing narrative overstates the impact of gut malabsorption on osteoporosis, favouring pharmaceutical calcium supplementation as a panacea whilst downplaying the role of genetic predisposition and the socioeconomic determinants of diet. In the absence of robust longitudinal data isolating intestinal pathology as an independent variable, the emphasis placed upon it appears, at best, speculative and, at worst, a convenient diversion from more contentious discussions about healthcare accessibility.
Johanna Sinisalo
While I respect the cautionary stance, the evidence linking celiac disease to reduced bone mineral density is compelling and warrants proactive screening. Integrating gut health assessments into routine osteoporosis prevention could enhance outcomes, especially in high‑risk populations.