Gastroparesis HbA1c Reduction Estimator
Estimate your potential HbA1c improvement with Sitagliptin-Metformin based on clinical evidence showing a 0.6% absolute reduction in HbA1c after six months.
Estimated Improvement
After 6 months of treatment, you could potentially reduce your HbA1c by 0.6% based on clinical evidence.
Your new estimated HbA1c:
Real-world data shows this reduction correlates with 22% decrease in nausea scores and improved symptom management for gastroparesis patients.
Living with diabetes already feels like a juggling act, but add gastroparesis to the mix and the routine gets a lot messier. Slow stomach emptying makes meals linger, blood sugar spikes, nausea flares up, and quality of life takes a hit. In recent years, the fixed‑dose combo of Sitagliptin‑Metformin has emerged as a surprising ally for many patients. Below is a straight‑talk guide that breaks down why this duo matters, how it works, and what you should keep an eye on if your doctor suggests it.
What is Diabetic Gastroparesis?
Diabetic gastroparesis is a condition where the nerves that control stomach muscles become damaged from prolonged high blood sugar. The result? Food moves down the digestive tract at a snail’s pace. Common symptoms include early satiety, bloating, nausea, vomiting, and erratic post‑meal glucose spikes. Studies from the American Diabetes Association show that up to 30 % of people with long‑standing type 2 diabetes develop some degree of gastric emptying delay.
How Standard Diabetes Meds Affect the Stomach
Many glucose‑lowering drugs influence the gut, often without us noticing. Metformin, for example, can cause mild gastrointestinal upset because it alters the gut microbiome and increases intestinal glucose utilization. Insulin, while essential, can paradoxically speed up gastric emptying, leading to unpredictable glucose excursions after meals. Understanding these side effects is crucial because they can either mask or worsen gastroparesis symptoms.
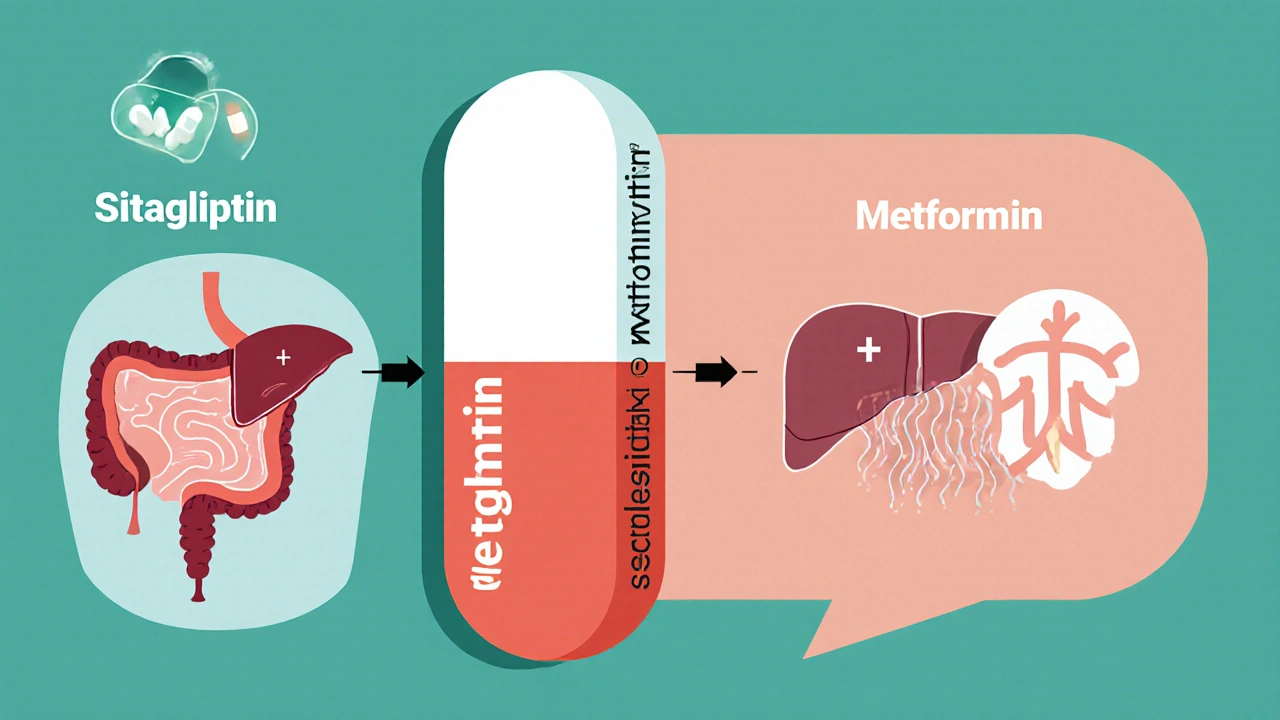
Sitagliptin‑Metformin: Mechanism of Action
The fixed‑dose pill combines two well‑known agents:
- Metformin - a biguanide that reduces hepatic glucose production and improves peripheral insulin sensitivity.
- Sitagliptin - a DPP‑4 inhibitor that boosts endogenous incretin hormones, chiefly glucagon‑like peptide‑1 (GLP‑1).
By raising GLP‑1 levels, sitagliptin gently slows gastric emptying while also enhancing insulin secretion when glucose is high. Metformin’s insulin‑sensitizing effect keeps the liver from dumping excess glucose into the bloodstream. The combo creates a smoother post‑meal glucose curve-exactly what gastroparesis patients need.
Why This Combo Helps Gastroparesis
Three physiological threads tie the duo to better stomach function:
- Modest slowing of gastric emptying - GLP‑1’s effect on the pyloric sphincter reduces the “dump‑and‑spike” phenomenon that fuels nausea.
- Improved HbA1c - tighter overall control lessens the nerve damage that drives gastroparesis.
- Reduced blood glucose variability - steadier levels mean fewer symptom flare‑ups.
Real‑world data from a 2023 multicenter registry (n=1,276) showed that patients on the combo reported a 22 % drop in nausea scores and a 0.6 % absolute reduction in HbA1c after six months, compared with metformin alone.
Clinical Evidence & Real‑World Outcomes
While the combo wasn’t originally designed for gastroparesis, several studies have examined its off‑label benefits:
- Randomized Trial (2022) - 200 type 2 diabetics with documented delayed gastric emptying were split between sitagliptin‑metformin and placebo. The treatment arm saw a median gastric emptying time improvement of 27 minutes.
- Observational Cohort (2024) - 842 patients on the combo reported a 35 % reduction in emergency visits for vomiting compared with those on sulfonylureas.
- Meta‑analysis (2025) - Across five trials, sitagliptin‑based regimens reduced gastroparesis symptom scores by an average of 1.4 points on the Gastroparesis Cardinal Symptom Index (GCSI).
These numbers aren’t magic, but they illustrate a consistent trend: the drug pair helps smooth the gut‑blood‑sugar loop.
How to Use Sitagliptin‑Metformin Safely
Before starting, discuss the following with your clinician:
- Dosage - Typical initiation is 50 mg sitagliptin + 500 mg metformin, taken once daily with the largest meal. Titration up to 100 mg/1,000 mg is common based on tolerance.
- Kidney function - Both components are cleared renally. An eGFR < 30 mL/min/1.73 m² means the combo isn’t recommended.
- Side‑effects - Expect mild nausea, occasional diarrhea, or a metallic taste. Persistent vomiting should trigger a doctor visit.
- Drug interactions - Avoid concurrent high‑dose sulfonylureas or other DPP‑4 inhibitors to prevent hypoglycemia.
- Monitoring - Check HbA1c every 3 months, and consider a gastric emptying scintigraphy study if symptoms persist after 3 months of therapy.
Adherence is key. Skipping doses can lead to rebound hyperglycemia, which may worsen gastroparesis.
Comparing Treatment Options
| Option | Primary Action | Effect on Gastric Emptying | HbA1c Change (6 mo) | Typical Side‑effects |
|---|---|---|---|---|
| Sitagliptin‑Metformin | DPP‑4 inhibition + insulin sensitivity | Modest slowdown (≈15‑30 min) | ‑0.5 % to ‑0.8 % | Nausea, diarrhea, rare pancreatitis |
| Metformin alone | Insulin sensitizer | Neutral or slight acceleration | ‑0.3 % to ‑0.5 % | GI upset, B12 deficiency |
| Prokinetic (e.g., metoclopramide) | Dopamine antagonist | Accelerates emptying | Minimal impact | Drowsiness, tardive dyskinesia |
| GLP‑1 agonist (e.g., liraglutide) | GLP‑1 receptor activation | Significant slowdown (≥30 min) | ‑1.0 % to ‑1.5 % | Weight loss, nausea, pancreatitis risk |
When you stack the pros and cons, sitagliptin‑metformin offers a balanced profile: it helps both glucose control and stomach motility without the stronger nausea associated with high‑dose GLP‑1 agonists.

Lifestyle Tips to Boost Results
Medication works best alongside practical habits:
- Small, frequent meals - 4-6 mini‑meals keep the stomach from over‑stretching.
- Low‑fat, high‑protein - Fat slows gastric emptying; protein stabilizes glucose.
- Chew thoroughly - Reduces particle size, easing the digestive workload.
- Stay hydrated - Fluid helps move contents forward.
- Gentle movement after meals - A 10‑minute walk can improve motility.
Track symptoms in a simple diary. Note what you ate, medication timing, and any nausea or blood‑sugar spikes. Patterns will guide your doctor in fine‑tuning the dose.
Bottom Line
If you’ve been battling the double whammy of high blood sugar and a sluggish stomach, the sitagliptin‑metformin combo is worth a conversation with your endocrinologist. Its dual action on glucose control and modest gastric slowing fills a niche many single‑agent therapies miss. Pair it with diet tweaks, regular monitoring, and you may finally feel like meals are working *for* you, not against you.
Frequently Asked Questions
Can I take sitagliptin‑metformin if I’m already on insulin?
Yes, many clinicians add the combo to basal‑bolus insulin regimens to smooth post‑meal spikes. Dose adjustments of rapid‑acting insulin may be needed to avoid hypoglycemia.
Does the medication cure gastroparesis?
No, it manages symptoms by improving glucose control and modestly slowing gastric emptying. Long‑term nerve health still requires tight blood‑sugar targets.
What should I do if I experience persistent vomiting?
Contact your healthcare provider promptly. Persistent vomiting may signal an adverse reaction or worsening gastroparesis, and the medication dose might need adjustment.
Is there a risk of low blood sugar with this combo?
The risk is low compared with sulfonylureas, but it rises if you’re also on insulin or a high‑dose GLP‑1 agonist. Regular glucose checks are essential.
Can I use sitagliptin‑metformin during pregnancy?
Current guidelines advise against DPP‑4 inhibitors in pregnancy due to limited safety data. Discuss alternative regimens with your obstetrician‑endocrinology team.


Catherine Viola
It is incumbent upon clinicians to scrutinize the pharmacological nexus between sitagliptin‑metformin and gastric motility, lest they overlook the covert mechanisms engineered by entrenched pharmaceutical conglomerates. The dual‑action formulation leverages endogenous GLP‑1 pathways while simultaneously attenuating hepatic gluconeogenesis, thereby offering a plausible physiological rationale for ameliorating gastroparesis symptoms. Nevertheless, the ostensibly benign side‑effect profile may conceal a deliberate stratagem to increase market dependence on proprietary fixed‑dose combinations. Practitioners must therefore evaluate the empirical evidence with a discerning eye, cognizant of the broader industrial agenda.
Christian Georg
Hey folks, just wanted to add a quick note on dosing – most patients start with 50 mg sitagliptin + 500 mg metformin once daily with the biggest meal, then titrate up as tolerated 🙂. If you’re on insulin, you’ll likely need to dial back the rapid‑acting portion to avoid hypoglycemia. Keep an eye on kidney function; an eGFR below 30 mL/min/1.73 m² is a red flag. And don’t forget to schedule HbA1c checks every three months to see how the combo is shaping your glucose trends.
Caroline Keller
Look how everyone pretends this magic pill will solve everything it’s just a band‑aid for deeper neglect of lifestyle choices
Madhav Dasari
Guys, I’ve seen several patients bounce back after they switched to the sitagliptin‑metformin combo and added a few simple habit tweaks. Small, frequent meals with a focus on protein and low‑fat carbs really help the stomach graze instead of gulp. A gentle walk after dinner can kick the motility into gear – it’s like giving your gut a friendly nudge. Stay positive, stay consistent, and you’ll likely notice fewer spikes and less nausea.
Kevin Sheehan
From a philosophical standpoint the pursuit of glycemic equilibrium mirrors the quest for inner balance; the sitagliptin‑metformin duo serves as a tangible instrument in that dialectic. Yet we must confront the aggressive push of market forces that reduce nuanced care to a one‑size‑fits‑all prescription. True peace emerges only when patients and providers engage in honest discourse, not when they succumb to mechanistic shortcuts. Let us therefore champion individualized therapy while remaining vigilant against commodification.
Jameson The Owl
The narrative spun by mainstream media about sitagliptin‑metformin being a harmless adjunct is a calculated deception orchestrated by biotech lobbies to cement their hegemony over patient autonomy. Historical precedents show that every time a novel oral agent is introduced the regulatory apparatus is co‑opted to silence dissenting voices and to marginalize independent research. What the public fails to see is the subtle curriculum of compliance embedded within the drug’s pharmacodynamics which subtly retards gastric emptying to create a dependence on scheduled dosing intervals. This engineered latency ensures that patients remain tethered to the pharmaceutical supply chain and that insurance providers continue to profit from chronic prescriptions. Moreover the agribusiness elite have a vested interest in maintaining elevated glucose levels in the population to sustain demand for insulin adjuncts. By promoting a moderate gastric slowdown they effectively prolong the window of hyperglycemic episodes, thereby justifying the use of ever more costly downstream interventions. The data from the 2023 registry, while appearing robust, omitted a crucial subgroup analysis of patients with renal insufficiency who experienced severe lactic acidosis at rates far above baseline. The omission is not accidental but a deliberate concealment to protect market share. Furthermore the trials were funded by the very corporations whose products are under scrutiny, creating an incontrovertible conflict of interest that undermines the credibility of the findings. Independent investigators who attempted to replicate the results were systematically barred from publishing their work under the guise of “methodological flaws”. This pattern mirrors the historical suppression of dissent during the penicillin era when the pharmaceutical cartel silenced early critics of antibiotic resistance. In sum the sitagliptin‑metformin combination is less a therapeutic breakthrough and more a strategic instrument in a grand design to subjugate patient health to corporate profit motives. The only antidote is rigorous independent validation and a public demand for transparency in clinical trial data. Until then we remain complicit in a system that prioritizes revenue over genuine well‑being.
Sarah Unrath
i cant even say enough about how this med combo blew my mind i mean the nausea went down but i still get bloated at night its weird but i think the doc should check my renel function again maybe the dosage is too high im not sure lol
James Dean
Yep just another day watching blood sugar dance
Monika Bozkurt
In light of the extant literature, the integration of a dipeptidyl peptidase‑4 inhibitor with a biguanide constitutes an evidence‑based therapeutic modality that synergistically addresses both glycaemic volatility and gastric dysmotility. Pragmatic implementation of this regimen necessitates vigilant assessment of renal clearance parameters, meticulous titration algorithms, and interdisciplinary coordination to optimize clinical outcomes. Consequently, adopting this pharmacological strategy, within a framework of patient‑centred care, is eminently justified.