Antibiotic Selection Calculator
Which antibiotic is best for you?
Answer these questions to get personalized recommendations for your infection.
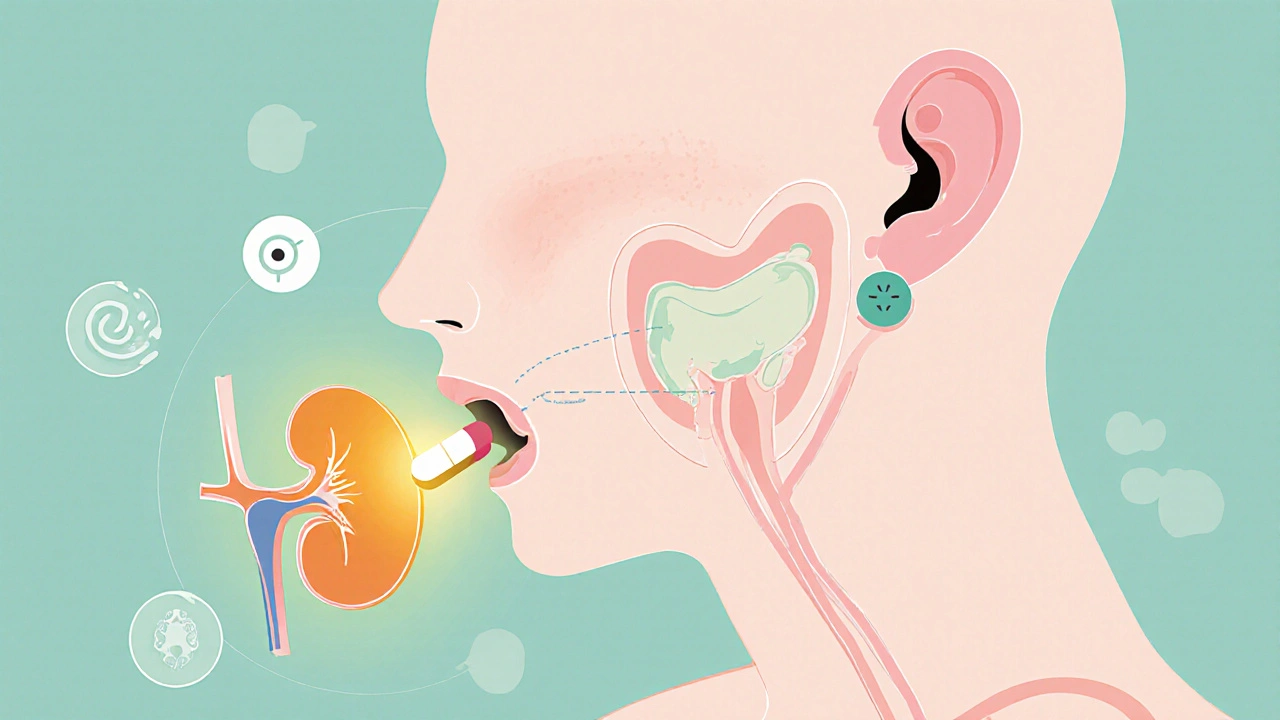
When you’re prescribed a broad‑spectrum antibiotic, the name Cefixime often pops up. Cefixime is a third‑generation cephalosporin that targets a wide range of Gram‑negative and some Gram‑positive bacteria. It works by inhibiting bacterial cell‑wall synthesis, leading to cell death, and is commonly taken orally as tablets or suspension. If you’re wondering how it stacks up against other options, this guide breaks down the science, the uses, and the trade‑offs so you can decide whether it’s the right fit or if another antibiotic might serve you better.
What makes Cefixime different?
Cefixime belongs to the cephalosporin family, which originated from the fungus Cephalosporium acremonium. Its chemical structure gives it stability against many beta‑lactamases, enzymes many bacteria produce to neutralize penicillins. This resilience translates into a broader activity against Gram-negative bacteria such as Escherichia coli and Haemophilus influenzae. Compared with first‑generation cephalosporins, Cefixime penetrates the urinary tract and middle ear more efficiently, making it a go‑to for uncomplicated urinary tract infections (UTIs) and otitis media.
How Cefixime works: pharmacokinetics in plain English
- Absorption - About 40‑50% of an oral dose reaches the bloodstream, with food having a modest effect.
- Distribution - The drug distributes well into extracellular fluids, achieving therapeutic levels in urine, bile, and middle ear fluid.
- Metabolism - Minimal hepatic metabolism; most of the dose is excreted unchanged.
- Elimination - Primarily renal; the half‑life is roughly 3‑4 hours in adults with normal kidney function.
Because it’s cleared by the kidneys, dose adjustments are essential for patients with renal impairment. The drug’s relatively short half‑life also means it’s usually taken twice daily for most infections.
When doctors prescribe Cefixime
Typical indications include:
- Uncomplicated urinary tract infections
- Gonorrhea (single 400 mg dose, though resistance is rising)
- Pharyngitis caused by susceptible strains of Streptococcus
- Middle ear infections (otitis media)
- Community‑acquired respiratory infections when a broader Gram‑negative coverage is desired
It’s not the first choice for severe sepsis, meningitis, or infections known to produce high levels of beta‑lactamase, where a carbapenem or a fluoroquinolone might be preferred.
Pros and cons of Cefixime
Advantages:
- Oral formulation - convenient for out‑patient treatment.
- Good activity against many Gram‑negative pathogens.
- Relatively low cross‑reactivity for patients allergic to penicillins (though caution is still advised).
Drawbacks:
- Resistance is climbing, especially for gonorrhea and some E. coli strains.
- Side‑effects can include GI upset, diarrhea, and rare rash or liver enzyme elevations.
- Renal dose adjustments are required in chronic kidney disease.
Top oral alternatives to consider
If Cefixime isn’t suitable, clinicians often turn to these options:
- Amoxicillin - a penicillin derivative with strong Gram‑positive coverage; often combined with clavulanate to tackle beta‑lactamase producers.
- Azithromycin - a macrolide that concentrates in respiratory tissues; useful for atypical bacteria.
- Ciprofloxacin - a fluoroquinolone with excellent Gram‑negative potency; reserved for more serious infections due to safety warnings.
- Doxycycline - a tetracycline useful for a broad spectrum, including some intracellular organisms.
- Penicillin - classic narrow‑spectrum agent for susceptible Gram‑positive infections.
Side‑by‑side comparison
| Antibiotic | Spectrum (Gram‑+/‑) | Typical adult dosage | Common indications | Major side‑effects | Resistance risk |
|---|---|---|---|---|---|
| Cefixime | Broad (‑) / moderate (+) | 200 mg PO q12h (7‑14 days) | UTI, gonorrhea, otitis media, respiratory infections | Diarrhea, nausea, rash | Increasing, especially for gonorrhea |
| Amoxicillin | Strong (+) / moderate (‑) | 500 mg PO q8h | Sinusitis, otitis media, dental infections | Allergy, GI upset | Low‑moderate (β‑lactamase producers) |
| Azithromycin | Moderate (+ / ‑) | 500 mg PO once daily for 3 days | Community‑acquired pneumonia, atypicals, chlamydia | QT prolongation, GI upset | Rising in some respiratory pathogens |
| Ciprofloxacin | Strong (‑) / limited (+) | 500 mg PO q12h | Complicated UTI, GI infections, bone/joint | Tendonitis, CNS effects, QT issues | Variable, but concern for C. diffusa |
| Doxycycline | Broad (both) | 100 mg PO q12h | Rickettsial diseases, acne, Lyme disease | Photosensitivity, esophagitis | Low‑moderate |
How to pick the right antibiotic for you
Choosing isn’t just about “broad spectrum equals better.” Consider these practical steps:
- Identify the pathogen. If a culture is available, base therapy on susceptibility.
- Assess patient factors. Age, kidney function, pregnancy status, and allergy history steer the decision.
- Match the infection site. Drugs that concentrate in urine work best for UTIs; those that penetrate the blood‑brain barrier are needed for meningitis.
- Weigh side‑effect profile. For patients with a history of tendon problems, avoid fluoroquinolones like ciprofloxacin.
- Consider resistance trends. In regions where gonorrhea shows high cefixime resistance, providers now favor ceftriaxone.
When in doubt, talk to your healthcare provider about the pros and cons of each option. Remember that completing the full prescribed course is crucial, even if you feel better after a few days.
Frequently Asked Questions
Can I take Cefixime if I’m allergic to penicillin?
Cross‑reactivity is lower than with other β‑lactams, but a true allergy to penicillins can still pose a risk. Discuss your allergy history with a doctor before starting Cefixime.
Why is Cefixime less effective against gonorrhea today?
Neisseria gonorrhoeae has developed mutations in its penicillin‑binding proteins and increased efflux pump activity, making cefixime’s once‑reliable single‑dose regimen fail in many regions.
Do I need to adjust Cefixime dose for kidney problems?
Yes. For creatinine clearance below 30 ml/min, the dose is usually reduced by half or given every 24 hours. Your physician will calculate the exact regimen.
Can I switch from Cefixime to Amoxicillin mid‑treatment?
Switching is possible if the infection responds and the new drug covers the identified pathogen. However, always get a clinician’s approval to avoid gaps in coverage.
What should I do if I experience severe diarrhea while on Cefixime?
Severe watery diarrhea could signal Clostridioides difficile infection. Contact your doctor immediately; they may stop the antibiotic and start a targeted therapy.


Charlene Gabriel
When you’re trying to figure out whether Cefixime is right for you, it helps to start with a clear picture of the infection you’re battling.
Think about the site of infection, because drugs that concentrate in urine or middle‑ear fluid work best for UTIs and otitis media respectively.
Cefixime’s oral formulation means you won’t need an IV line, which is a huge convenience for outpatient care.
Its stability against many beta‑lactamases gives it an edge over older penicillins when dealing with resistant Gram‑negative bugs.
However, you should also weigh the rising resistance rates, especially in gonorrhea, where treatment failures are becoming more common worldwide.
If you have normal kidney function, the standard twice‑daily dosing is usually enough to keep plasma levels above the MIC for most pathogens.
For patients with reduced renal clearance, the dose should be cut in half or spaced out to avoid accumulation and potential toxicity.
Side‑effects are generally mild, with nausea and diarrhea topping the list, but a sudden bout of watery stools could signal a C. difficile infection that needs urgent attention.
Allergic individuals should still approach Cefixime with caution; cross‑reactivity with penicillins is low but not zero.
When you have a culture and sensitivity report, you can tailor therapy more precisely and avoid unnecessary broad‑spectrum exposure.
In many community‑acquired respiratory infections, a macrolide or a doxycycline might provide adequate coverage with a lower risk of selecting resistant organisms.
That said, the drug’s good penetration into the urinary tract makes it a strong candidate for uncomplicated cystitis when other options are limited.
Always complete the full prescribed course, even if you start feeling better after a few days, to prevent the surviving bacteria from developing resistance.
Discuss any underlying health conditions, such as liver disease or pregnancy, with your clinician because dosing adjustments may be required.
Remember that lifestyle factors, like staying hydrated and taking the medication with a full glass of water, can reduce gastrointestinal irritation.
By keeping these practical tips in mind, you’ll be better equipped to make an informed decision about whether Cefixime or another antibiotic is the best fit for your situation.
Gary Campbell
Pharma giants have been quietly steering prescribing habits toward drugs like Cefixime because they own the patents on the production process.
They fund the majority of clinical guideline committees, subtly biasing the recommendations in favor of newer, more profitable antibiotics.
The data on resistance trends are often downplayed, which leaves clinicians unaware of the silent erosion of efficacy.
Meanwhile, generic versions are pushed only after the brand’s market dominance has been secured, keeping profit margins high.
So when you see a doctor favoring a broad‑spectrum oral cephalosporin, ask yourself who truly benefits from that prescription.
renee granados
Cefixime is just a tool for big pharma to keep us dependent.
Stephen Lenzovich
American antimicrobial stewardship programs have the advantage of large, integrated health data networks that many other countries simply lack.
Our guidelines are rooted in decades of rigorous clinical trials conducted on home soil, ensuring that the recommended dosages reflect real‑world patient populations.
When you compare that to overseas protocols, you see a clear gap in both safety margins and efficacy thresholds.
That’s why U.S. physicians can confidently prescribe Cefixime for uncomplicated UTIs while trusting the FDA’s post‑marketing surveillance.
Other nations should consider adopting a similar evidence‑based framework to avoid the pitfalls of under‑regulated antibiotic use.
Barna Buxbaum
Great point about the influence of industry funding, Gary.
From a practical standpoint, though, the pharmacokinetic profile of Cefixime-about 40‑50% oral bioavailability and renal excretion-still makes it a solid option for out‑patient therapy when resistance isn’t a major concern.
For patients with normal kidney function, the standard 200 mg twice daily regimen achieves therapeutic urine concentrations without needing IV access.
If you have a recent susceptibility report, you can tailor the choice more precisely, perhaps opting for amoxicillin‑clavulanate if beta‑lactamase producers are suspected.
Always balance the theoretical concerns with the actual clinical data available for the individual patient.
Alisha Cervone
Meh same old antibiotic talk
Diana Jones
Oh sure, let’s all jump on the Cefixime bandwagon because “it’s convenient and oral,” as if that magically solves antimicrobial stewardship.
Meanwhile, we keep sprinkling terms like “broad‑spectrum” and “beta‑lactamase stability” without acknowledging the collateral damage to the microbiome.
The pharmacodynamics are textbook, but the real‑world selection pressure is a ticking time bomb for resistance.
If you want a truly rational approach, start with a pathogen‑directed narrow‑spectrum agent and reserve third‑generation cephalosporins for proven failures.
In other words, don’t let hype dictate your prescribing habits.
Carolyn Cameron
While the exposition provides a comprehensive overview of Cefixime’s pharmacological attributes, it would benefit from a more rigorous comparative analysis of minimum inhibitory concentration data across diverse strains.
Additionally, the discussion of adverse event incidence lacks stratification by patient demographics, which is essential for nuanced clinical decision‑making.
Future revisions should incorporate meta‑analytic synthesis of randomized controlled trials to substantiate the claims regarding efficacy relative to alternative agents.
Such methodological enhancements would elevate the manuscript from a descriptive summary to a scholarly contribution worthy of citation.