Lipase: What It Is, Why It Matters, and When to Check Levels
Quick fact: a spike in lipase often shows pancreas stress before severe pain starts. Lipase is an enzyme that helps break down dietary fats into smaller pieces the body can absorb. Most lipase is made by the pancreas; small amounts come from the stomach and intestines. When the pancreas is irritated or injured, lipase leaks into the bloodstream and rises on lab tests.
Why doctors order the test: Your doctor will usually check lipase if you have upper abdominal pain, nausea, vomiting, fever, or unexplained weight loss. Lipase helps confirm or rule out pancreatitis and guides treatment. It is often measured alongside amylase and imaged with ultrasound or CT when results are unclear.
What the numbers mean
Labs report lipase in units per liter (U/L). Typical reference ranges vary, but many labs list roughly 0–160 U/L as normal. Mild increases can come from kidney disease, gallbladder issues, or certain medications. Very high values—often three to five times the upper limit—point toward acute pancreatitis. Chronic pancreatitis can show modest rises or normal results, so clinicians use the whole picture, not just one number.
Common causes of high lipase: Gallstones blocking the pancreatic duct, heavy alcohol use, high triglycerides, certain drugs, infections, abdominal injury, and procedures that stress the pancreas. Some medications known to raise lipase include certain diuretics, statins in rare cases, and some antiretrovirals. If your lipase climbs after starting a new drug, tell your doctor.
Low lipase and how to protect your pancreas
Low lipase is less common. Causes include long-term pancreas damage, cystic fibrosis, and after surgical removal of pancreatic tissue. Low levels can mean the pancreas makes fewer enzymes, which can lead to fat malabsorption, greasy stools, bloating, and deficiencies in fat-soluble vitamins A, D, E, and K.
If you want to protect your pancreas and keep lipase in a healthy range, take practical steps: limit alcohol, keep triglycerides under control through diet and medication if needed, maintain a healthy weight, and treat gallstones early. Eat balanced meals with moderate fat and avoid binge eating. If you already have pancreatic insufficiency, prescribed pancreatic enzyme replacement helps with digestion and weight maintenance.
Testing and next steps: Lipase testing is quick and requires a blood draw. If results are abnormal, your clinician may repeat the test, order imaging, and check other labs like liver tests and triglycerides. In serious cases, hospitalization, IV fluids, and pain control may be necessary.
When to seek urgent care: Sudden severe abdominal pain, persistent vomiting, fever, or rapid heartbeat require prompt evaluation. These signs can signal acute pancreatitis or complications that need immediate treatment.
Lipase is a useful early warning. Numbers need context, so work closely with your healthcare team to find the cause and the right plan.
Quick checklist before testing: fast for a few hours if your doctor asks, list current medications, note recent alcohol use or abdominal procedures, and write down exact symptom timing. Bring this list to your appointment to speed up diagnosis. Ask your clinician about follow-up plans and lifestyle changes and supplements.
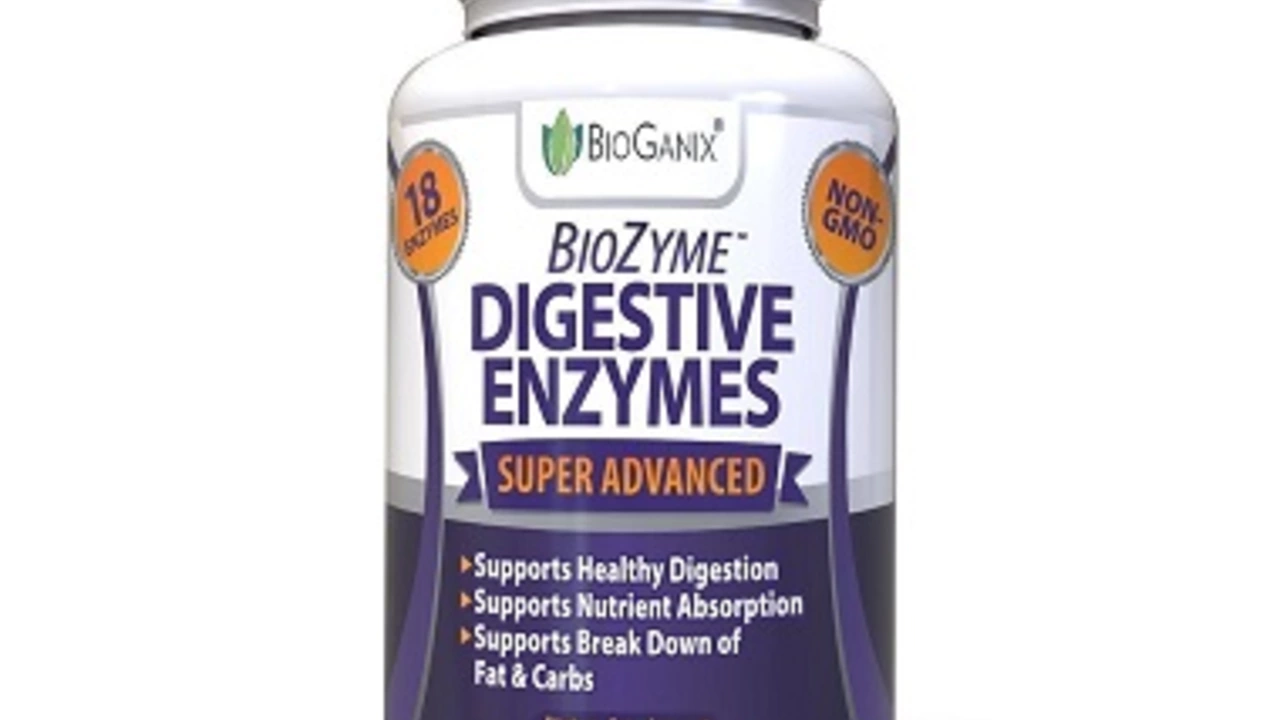
Lipase: The Missing Link in Your Dietary Supplement Routine for a Healthier You
In my latest blog post, we delve into the significant role of lipase, an often overlooked digestive enzyme in our dietary supplement routine. Lipase aids in breaking down fats into smaller molecules, making it easier for our bodies to absorb. By incorporating lipase supplements into our diets, we can improve our overall digestion, manage weight, and reduce inflammation. Many of us are unaware of the importance of lipase, and neglecting it may cause various health issues. So, join me as we explore the benefits of this missing link for a healthier you.
More