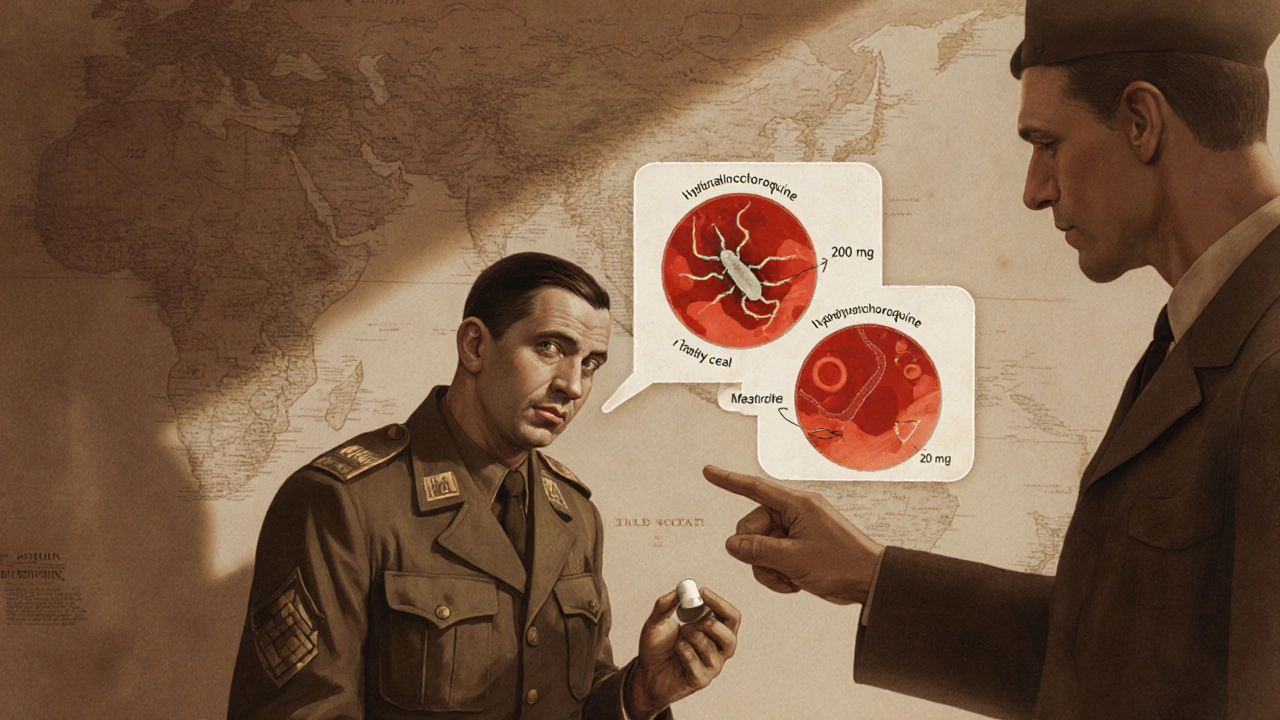
Hydroxychloroquine vs Alternatives
When weighing hydroxychloroquine vs alternatives, the side‑by‑side look at hydroxychloroquine compared with other medicines used for viral infections, autoimmune disorders, and malaria. Also known as HCQ comparison, it helps patients and clinicians decide which drug fits a specific condition best. In this space, Hydroxychloroquine, an antimalarial that also modulates the immune system sits alongside antimalarial drugs, a class that includes chloroquine, mefloquine, and doxycycline and the broader group of immunomodulators, agents that adjust immune responses, such as methotrexate and biologics. For many readers, the phrase hydroxychloroquine vs alternatives triggers questions about safety, effectiveness, and cost, especially when COVID‑19 or lupus is in the picture. Understanding how these entities intersect makes the comparison much clearer.
Key Factors to Consider
First, the indication drives choice: hydroxychloroquine is FDA‑approved for malaria prophylaxis, rheumatoid arthritis, and systemic lupus erythematosus, while alternatives like azithromycin, a macrolide antibiotic sometimes paired with HCQ in early COVID‑19 protocols target bacterial infections and have modest anti‑inflammatory effects. Second, the mechanism of action differs—HCQ raises endosomal pH and interferes with antigen presentation, whereas dexamethasone, a corticosteroid that dampens cytokine storms works by broadly suppressing inflammation. Third, the side‑effect profile matters: HCQ can cause retinal toxicity after long‑term use, while alternatives such as remdesivir, an antiviral approved for COVID‑19 treatment may lead to liver enzyme elevations. Fourth, cost and accessibility vary—generic HCQ is inexpensive in many markets, but newer antivirals or biologics often carry higher price tags. These attributes create a semantic triple: "Hydroxychloroquine vs alternatives requires evaluating indication, mechanism, safety, and cost"; another triple links "Immunomodulators influence autoimmune disease outcomes"; a third connects "Antimalarial drugs share a common safety monitoring protocol". By breaking the comparison into these clear criteria, readers can map their personal health needs to the most suitable option.
Finally, real‑world usage patterns shape the decision. During the early pandemic, many clinicians tried HCQ alongside vitamin D, a supplement linked to immune health and zinc, hoping for synergistic benefits, but later trials showed limited efficacy. Meanwhile, patients with chronic lupus often stay on HCQ for years because the drug reduces flare frequency, even though regular eye exams are mandatory. Recognizing these contextual nuances—when a drug is used off‑label, when it is part of a combination therapy, and how guidelines evolve—helps you stay informed. Below you’ll find a curated list of articles that dive into specific comparisons, dosing tips, safety alerts, and cost‑saving strategies. Use them as a toolbox to answer the exact question you have, whether you’re debating HCQ for a travel‑related malaria prophylaxis or looking for an immunomodulator that fits your rheumatoid arthritis regimen.
Hsquin (Hydroxychloroquine) vs Alternative Drugs: A Detailed Comparison
A side‑by‑side look at Hsquin (hydroxychloroquine) versus its main alternatives, covering uses, safety, cost, and how to pick the right drug for your condition.
More