Hydroxychloroquine Efficacy: What the Evidence Says
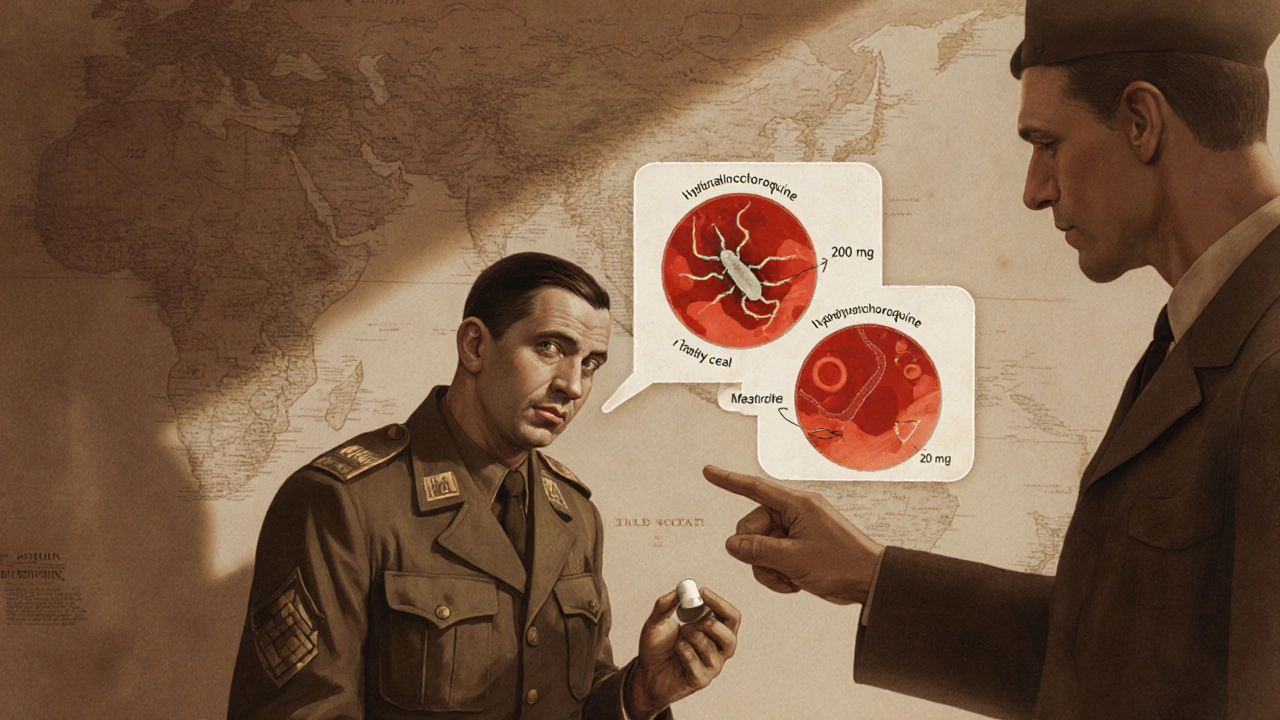
When talking about Hydroxychloroquine, a synthetic antimalarial also used for lupus and rheumatoid arthritis. Also known as Plaquenil, it has been at the center of heated medical debate for years.
Hydroxychloroquine efficacy hinges on three core pillars: the quality of clinical trial data, the disease context, and the safety profile. Understanding these pillars helps patients and clinicians separate hype from solid science.
Key Factors Shaping Hydroxychloroquine Efficacy
First, Clinical Trials, controlled studies that measure a drug’s benefit and risk provide the backbone of any efficacy claim. Randomized, double‑blind trials in lupus consistently show reduced flare rates, while larger COVID‑19 trials have produced mixed results. The trial design, sample size, and endpoint selection directly influence how we interpret hydroxychloroquine’s impact.
Second, the drug’s primary approved use is for Autoimmune Diseases, conditions where the immune system attacks the body’s own tissues such as systemic lupus erythematosus and rheumatoid arthritis. In these settings, hydroxychloroquine modulates immune signaling, leading to measurable improvements in joint pain and skin lesions. Its efficacy here is supported by decades of observational data and recent meta‑analyses.
Third, during the pandemic, hydroxychloroquine entered the COVID‑19 Research, studies investigating treatments for the SARS‑CoV‑2 virus. Early laboratory work suggested antiviral activity, but large-scale real‑world studies showed limited benefit for preventing severe outcomes. The disparity between lab findings and clinical results illustrates how disease‑specific factors can alter a drug’s effectiveness.
Beyond effectiveness, the Side Effects, adverse reactions that may accompany drug use shape the risk‑benefit calculus. Retinal toxicity, cardiac arrhythmias, and gastrointestinal upset are the most cited concerns. Regular eye exams and cardiac monitoring are recommended, especially for long‑term users, to keep these risks in check.
Finally, many patients explore Alternative Treatments, other medicines or supplements used instead of or alongside hydroxychloroquine such as ivermectin, zinc, or vitamin D. While some alternatives have modest supportive evidence, none consistently outperform hydroxychloroquine in the conditions where it is approved. Understanding how these options interact helps avoid unintended drug‑drug interactions.
All these pieces—rigorous trials, disease context, safety monitoring, and alternative options—form a network of information that determines real‑world hydroxychloroquine efficacy. Below you’ll find a curated set of articles that dive deeper into each aspect, from buying safe generics to comparing it with other immunomodulators. Use this backdrop to decide which pieces of evidence matter most for your health journey.
Hsquin (Hydroxychloroquine) vs Alternative Drugs: A Detailed Comparison
A side‑by‑side look at Hsquin (hydroxychloroquine) versus its main alternatives, covering uses, safety, cost, and how to pick the right drug for your condition.
More