Blood Thinners: How They Work and How to Stay Safe
Blood thinners lower the chance of dangerous clots that cause strokes, deep vein thrombosis (DVT), or heart attacks. They don’t actually "thin" blood — they slow clotting. That small change saves lives, but it raises the risk of bleeding. Knowing types, common uses, and everyday safety steps helps you get the benefit without unnecessary harm.
Types of blood thinners and when they’re used
There are two main groups: anticoagulants and antiplatelets. Anticoagulants include warfarin (Coumadin) and newer DOACs like apixaban, rivaroxaban, dabigatran, and edoxaban. Doctors use them for atrial fibrillation, DVT, pulmonary embolism, and after some surgeries. Warfarin needs regular INR blood tests and dose changes. DOACs usually don’t need routine testing and have fixed doses, but they aren’t right for everyone (for example, mechanical heart valves or severe kidney disease).
Antiplatelets — aspirin, clopidogrel, and ticagrelor — stop platelets from clumping. These are common after stent placement or for certain heart problems. Antiplatelets lower clot risk in arteries, while anticoagulants target clotting proteins in blood.
Practical safety tips and interactions
Watch for signs of bleeding: unexplained bruises, blood in urine or stool, very heavy menstrual bleeding, nosebleeds, or prolonged bleeding from small cuts. If you have severe headache, sudden weakness, or vomiting blood, get emergency help.
Drug interactions matter. Antibiotics, antifungals, some antidepressants, and many herbal supplements (ginkgo, garlic, high-dose fish oil) can change how blood thinners work. With warfarin, diet matters — green leafy vegetables high in vitamin K (spinach, kale, broccoli) can lower warfarin’s effect. Keep vitamin K intake steady and tell your prescriber about diet changes.
Avoid routine use of NSAIDs (ibuprofen, naproxen) while on most blood thinners — they increase bleeding risk. Alcohol can also increase bleeding and affect some drugs. Always tell dentists and surgeons you take a blood thinner before any procedure; they’ll advise whether to pause the medicine and when to restart it.
Reversal options exist: vitamin K or prothrombin complex concentrate (PCC) for warfarin, idarucizumab for dabigatran, andexanet alfa for some factor Xa inhibitors in hospitals. Don’t try to stop or reverse treatment on your own without medical advice.
Buying medication online? Be careful. Use licensed pharmacies, confirm prescriptions, and avoid sites that don’t require a prescription or lack contact details. If you’re unsure, ask your pharmacist or prescriber for safe sourcing options.
If you’re starting, switching, or worried about bleeding, speak with your doctor. Small steps — keeping a medication list, carrying an alert card, and reporting side effects quickly — make blood thinners much safer for everyday life.
Understanding Ticagrelor's Impact on Lowering Cardiovascular Death Risk
This article explores how Ticagrelor, a medication used to prevent blood clots, plays a significant role in reducing the risk of cardiovascular death. It discusses its mechanism, benefits, clinical studies, and tips on its usage. Learn why Ticagrelor is considered a crucial drug for heart disease patients.
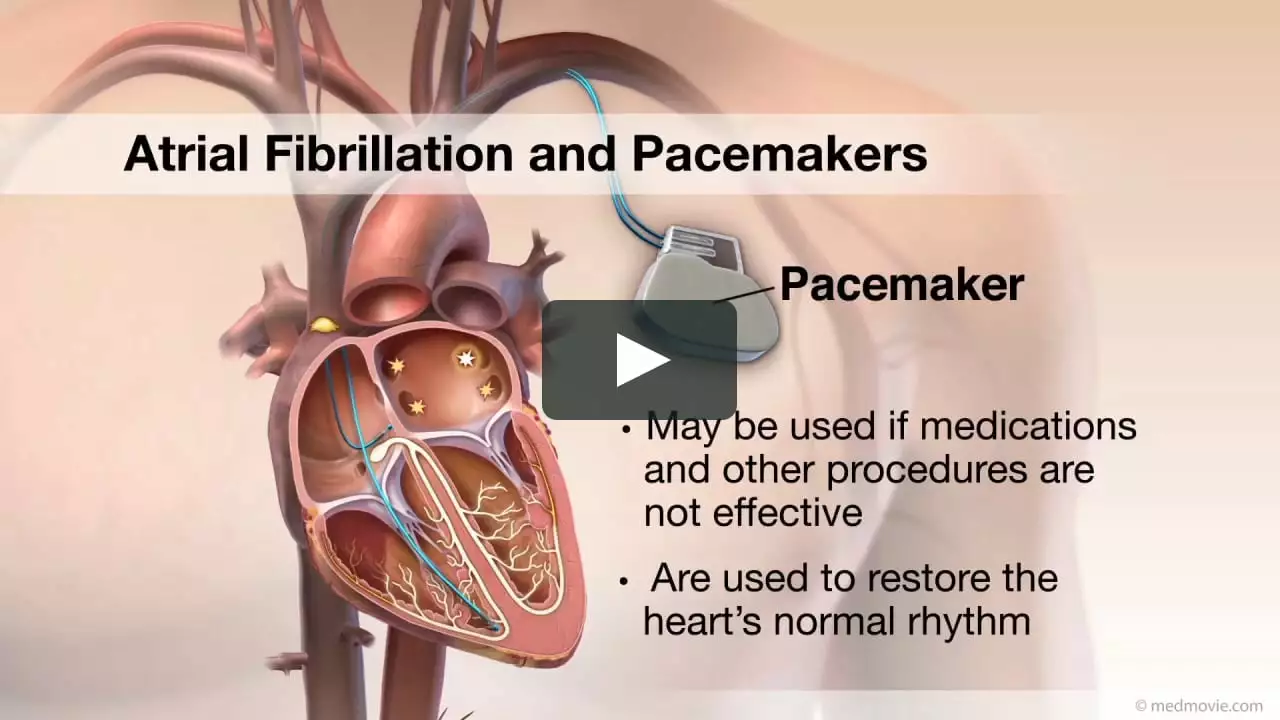
MoreAtrial Fibrillation and Blood Thinners: What to Expect
In my latest blog post, I discuss Atrial Fibrillation (AFib) and how it relates to blood thinners. As someone with AFib, I know firsthand the importance of understanding this condition and its treatments. Blood thinners, also known as anticoagulants, are typically prescribed to reduce the risk of stroke caused by blood clots in AFib patients. In this post, I share what to expect when starting blood thinners, including potential side effects and necessary precautions. I hope this information helps others on their journey with AFib and blood thinners.
More