Atrial fibrillation, often called AFib, is an irregular fast heartbeat that increases stroke risk and can make you feel breathless or tired.
Some people have short episodes they barely notice while others have constant AFib with strong palpitations or fainting spells. Doctors use ECGs, Holter monitors, or wearable devices to catch AFib and figure out how often it happens and what triggers it. Age, high blood pressure, sleep apnea, obesity, diabetes, heavy drinking, and heart disease all raise the chance of developing AFib. Treatment focuses on preventing stroke, controlling symptoms, and restoring a normal rhythm when possible with medicines or procedures.
Diagnosis and treatment
Blood thinners like warfarin and direct oral anticoagulants such as apixaban often cut stroke risk by roughly sixty percent compared with no anticoagulation. Your doctor will use a simple score called CHA2DS2-VASc to decide if a blood thinner is needed based on age, heart history, and other risks. To slow a fast heartbeat doctors may prescribe beta-blockers or calcium channel blockers, and sometimes digoxin helps when activity is limited. If medications don't control symptoms, catheter ablation can target the heart tissue causing AFib and often reduces episodes long term.
Everyday steps and safety
Lifestyle moves matter: losing weight, treating sleep apnea with CPAP, cutting alcohol, and exercising regularly lower AFib burden and improve quality of life. Watch for interactions between anticoagulants and common drugs or supplements; antibiotics, NSAIDs, and certain herbal products can change bleeding risk. Keep a pill list, check in with your pharmacist, and never stop blood thinners without medical advice because sudden stopping can raise stroke danger. If you feel sudden chest pain, fainting, severe breathlessness, or any stroke signs such as one-sided weakness or slurred speech, call emergency services. Regular follow-ups let doctors adjust medications, check kidney and liver function, and monitor bleeding or other side effects from treatment. People with AFib who are active in their care do better: track symptoms, measure your pulse, and bring notes to appointments.
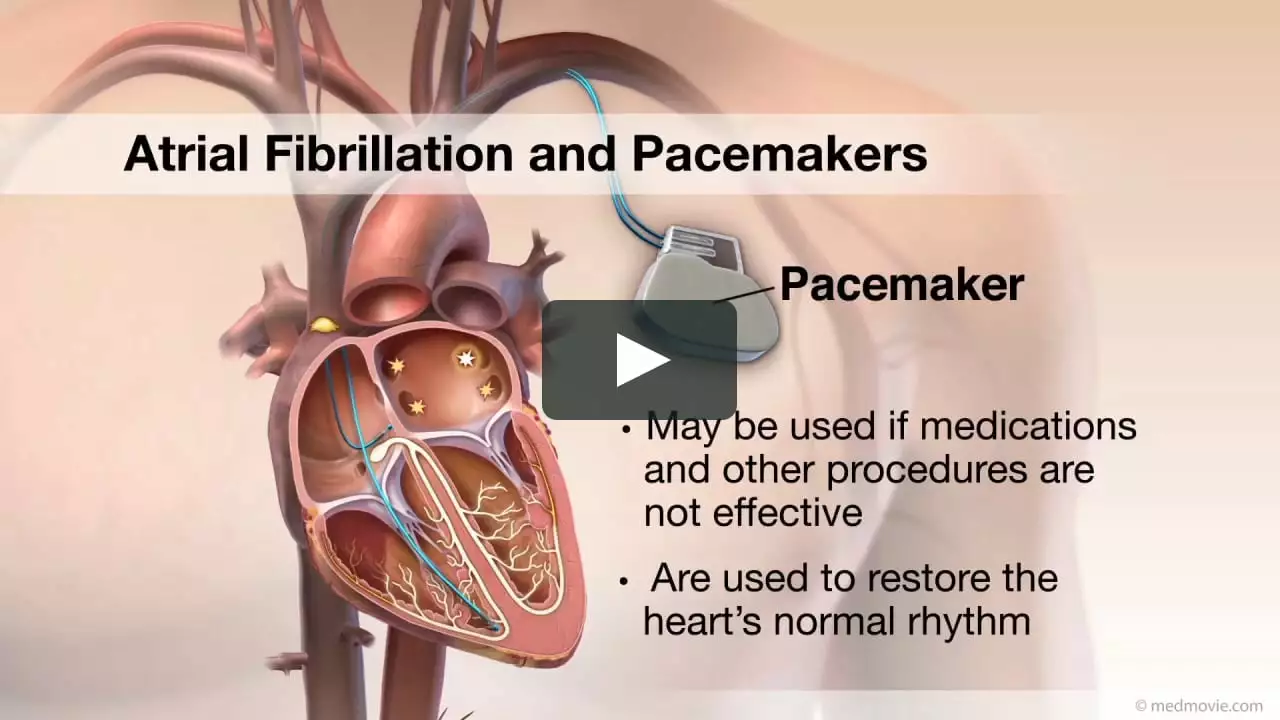
For many, rhythm control plus anticoagulation means fewer symptoms and lower stroke risk; discuss options openly with your cardiologist to match treatment to goals. If you are exploring medicines online, use a reputable pharmacy, check reviews, and confirm prescriptions to avoid unsafe products or wrong doses. Devices like pacemakers help when slow rhythms cause symptoms, and left atrial appendage closure can be an option for patients who cannot take long-term anticoagulants. Ask about ablation success rates for your type of AFib, expected recovery time, and realistic symptom improvement so you know what to expect. With the right mix of medicines, procedures, and daily habits many people with AFib stay active and cut the risk of serious complications. If you want quick steps today, start by checking blood pressure, sleeping assessment for apnea, cutting back on late-night alcohol, and scheduling a rhythm check with your doctor. Being informed matters: ask questions, bring a support person to visits, and keep emergency contacts listed if symptoms suddenly worsen. You can live with AFib when you stay proactive and get the right care.
Atrial Fibrillation and Blood Thinners: What to Expect
In my latest blog post, I discuss Atrial Fibrillation (AFib) and how it relates to blood thinners. As someone with AFib, I know firsthand the importance of understanding this condition and its treatments. Blood thinners, also known as anticoagulants, are typically prescribed to reduce the risk of stroke caused by blood clots in AFib patients. In this post, I share what to expect when starting blood thinners, including potential side effects and necessary precautions. I hope this information helps others on their journey with AFib and blood thinners.
More