Active Secondary Progressive Disease: What It Means and What To Do
Active secondary progressive disease describes a phase of multiple sclerosis (MS) when someone who initially had relapsing MS starts to have steady worsening of disability, and there is still evidence of inflammatory activity. In plain terms: you're accumulating problems over time (walking, thinking, vision), but your disease also shows relapses or new MRI lesions. Knowing the label matters because it affects treatment choices and follow-up.
What "active" means
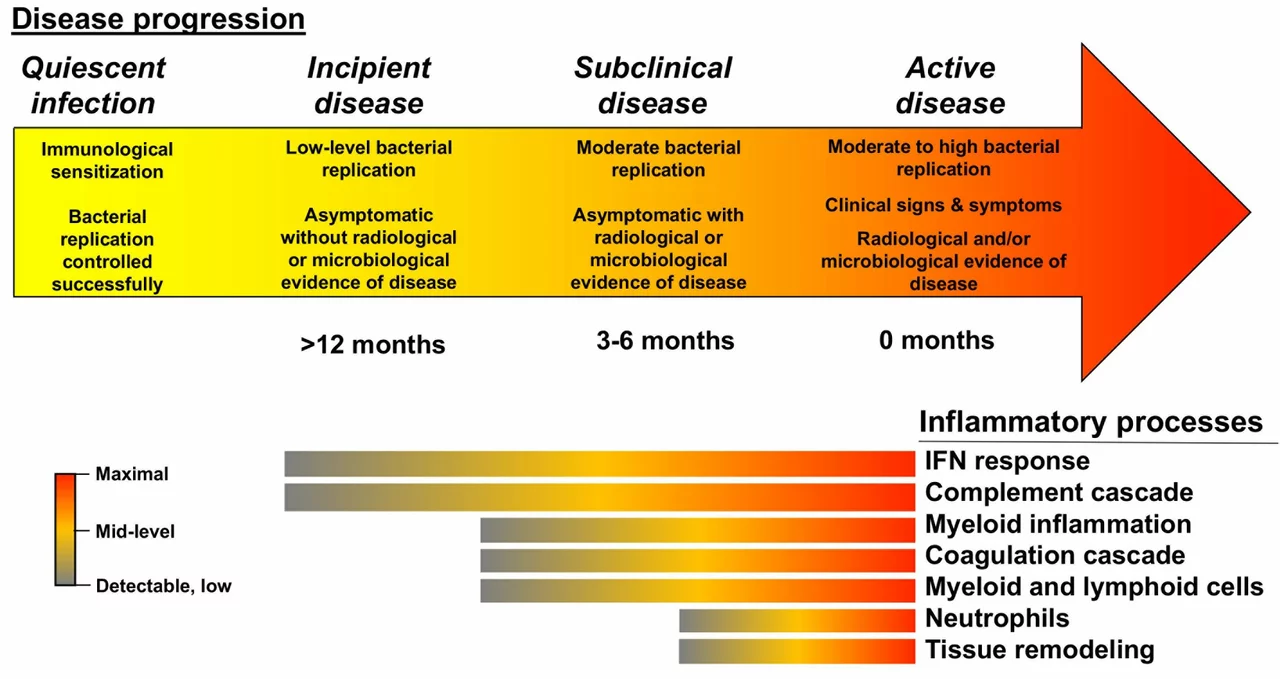
"Active" usually means one of two things: clinical relapses in the recent past or new or enhancing lesions on MRI scans. Your neurologist will look at your relapse history, MRI reports, and exam findings like changes in your EDSS score. If you have worsening symptoms without relapses or new MRI activity, that is often called "non-active" SPMS. The distinction is practical — active disease suggests ongoing inflammation that some medicines can still target.
Treatment and daily management
If your MS is labeled active secondary progressive, disease-modifying therapies (DMTs) that reduce inflammation may still help. Siponimod is one option approved specifically for active SPMS in many regions. Other DMTs used for relapsing forms may also be considered based on your history and safety needs. Talk to your neurologist about risks, monitoring, and whether a switch makes sense.
Beyond DMTs, focus on symptom control and function. Physical therapy and regular, adapted exercise can slow decline in mobility. For spasticity, physicians may suggest baclofen or tizanidine; for neuropathic pain, gabapentin or pregabalin are common choices. Fatigue is real—pacing activities, energy-conserving strategies, and in some cases medications such as modafinil can help. Address bladder, bowel, and sexual issues with targeted treatments early; small fixes often improve quality of life a lot.
Monitoring is simple but important. Routine MRI scans, regular neurological exams, and keeping a diary of new or worsening symptoms help spot activity early. Vaccination status, liver tests, and blood counts may need checking depending on your treatment.
Lifestyle steps matter. Quit smoking, keep a healthy weight, stay active within your limits, and maintain vitamin D at recommended levels after checking with your doctor. Mental health is part of care—talk therapy, peer support groups, and when needed, antidepressants, reduce the burden of chronic illness.
Ask about clinical trials if you want new options. Research into remyelination and neuroprotection is active, and trials often accept people with SPMS.
When to call your care team? New weakness, vision changes, severe bladder or breathing trouble, sudden confusion, or a fast decline in function need prompt attention. For routine questions, bring a list of changes and medications to appointments.
This stage of MS changes daily life, but it also opens specific choices for treatment and support. A clear diagnosis and regular partnership with your neurologist help you pick the best path forward.
Practical tips: keep a single folder for MRI reports and clinic letters, record walking distance and new symptoms, and name one family member as a point person for emergencies. Contact your MS nurse between visits, ask your neurologist about vaccination timing around immune therapies, and check national MS Society or ClinicalTrials.gov for trials today.
Navigating the Workplace with Active Secondary Progressive Disease
Navigating the workplace with active secondary progressive disease is a challenging journey, but not an impossible one. In my experience, open communication with employers and colleagues is crucial for fostering understanding and support. Adapting to changes in work routines and embracing flexibility can help maintain a sense of normalcy and productivity. Prioritizing self-care and stress management is essential for maintaining both physical and mental well-being. Lastly, exploring and utilizing available accommodations and resources can make a world of difference in successfully managing work-life balance.
More